- Joined
- Jun 8, 2008
- Messages
- 56,765
"

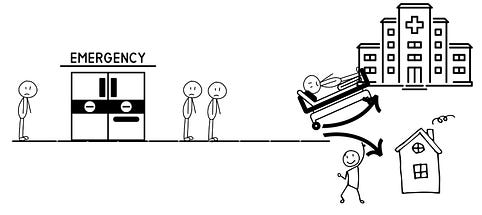
Now that patients have online access to their medical information there have been several articles and posts published recently about the increase in patientsopens in a new tab or window seeking -- in real time -- information and explanations about clinical results appearing on their charts. There are also reports now appearing noting that many healthcare facilities are increasingly seeking to billopens in a new tab or window patients for these interactions.
Growing Work Loads: A Case Study
I have been working with one physician colleague concerning evolving changes in his long-standing healthcare workplace and his accelerating feelings of frustration, burnout, and dissatisfaction.
He tells me now that a "final straw" has just been added: real-time health portal messages.
He reports that he used to derive satisfaction from his work, feeling that he was helping people -- the reason, he states, that he sought a career in healthcare. However, the evolving changes in his long-time workplace have now essentially destroyed all that.
Over time, he's seen other changes to his workplace too. The changes began when the facility switched physician contracts to "employee" status. Shortly after, his clinic administrator upped the cap on the number of allowable clinical patient evaluations, first from 4 to 5 per hour and more recently, up to 6 per hour. He told me the per hour cap was originally set based on the complexity and type of patient seen in this clinic. However, in his view the higher caps appear to be an attempt by the facility to increase revenue.
Within the 6 per hour, he reports that usually one to two are new patient evaluations. The facility administration has additionally announced that they expect the majority of interactions to be billed as a "level 3" (or higher).
(A level 3 clinical established follow-up has a typical time of 15 minutesopens in a new tab or window with an actual performance range of 20-29 minutes in 2021, and a new patient E/M level 3 typical time is 30 minutes with the 2021 range averaging 30-44 minutes.)
Six patients each at 15 to 29 minutes per patient, per each 60 minutes? You do the math.
While it's true that administrators frequently overbook clinic visits due to no-show patients who then leave holes in the schedule, this particular clinic has always had a very low percentage of no-shows. This patients per hour computation also does not factor in any additional time for any procedures that might have to be performed.
The physician is also expected, during these time periods, to periodically walk over to an adjacent clinic area to interact with and review the progress of the NP that he is now required to supervise.
He reports that moving to a six patients/hour schedule with these parameters and NP coverage has significantly degraded his ability to keep up, and he reports that his administrator told him recently that she was forced to report him for the increasing delays in patients being seen in a timely fashion in his clinic.
He has attempted multiple times to voice his concerns about these changes to the facility leadership through the appropriate channels, but has not yet even received an acknowledgement, much less a reply to his concerns.
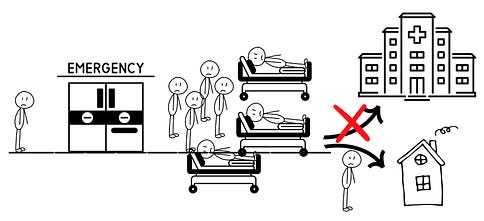
Now, on to the "last straw." Recently, increasing numbers of patients phone calls have been coming into the clinic related to lab tests, imaging studies, and other performance data that this clinic's patients can now access online.
As the number of calls increase and as the facility investigates "billing" for these interactions, he reports that the facility has decided he needs to answer these calls "in real time" as they come in, and take whatever time necessary to fully explain lab and test results to these patients.
Previously, before returning these calls, he had been trying to review and familiarize himself with the report results such as lab tests, or other imaging studies that have been queried -- especially if the results might provide bad news. He would return these calls after his last on-site patient left the clinic, along with the multiple preauthorization peer-to-peer calls he is required to perform with insurance companies.
Yet, despite the new demand to respond right away, he has not been given more time in the clinical schedule to review the information or take the calls. He is still being held to the 6 patients/hour time frame -- and being dinged when he falls behind.
He finds the new approach to these calls profoundly stressful for both him and the patient, and they are leading to distraction and potential loss of focus when he returns to the next on-site patient waiting to be seen. He's concerned this distraction could contribute to medical errors.
He has also tried to share his concerns about increased medical risks with the administration -- but again, with no response.
A Dwindling Workforce
The combination of the increase in patients-per-hour, supervision of mid-level personnel, and now patients calling in during clinical time for results has become, for him, the last straw.
In evaluating his current options, he is not able to migrate to other geographically local facilities due to a non-compete clause he was required to sign when the practicing physicians at his facility were converted to "employee" status, with facilities aggressively attempting to enforce such clauses in his locale.
So, while he felt he was in a previously successful mid-career timeline, he is now considering leaving clinical practice and moving into a non-patient care setting -- or even non-medical setting.
Another good physician (with excellent patient reviews and performance ratings) chewed up by the dystrophic, toxic healthcare workplace. Of course, he's not alone -- too many other doctors and nurses likely feel similarly.
So, it's surprising to me that I am increasingly asked on a regular basis why more and more doctors and nurses are quitting healthcare and why the specter of unionization is starting to appear in the healthcare workplace.
Harry Severance, MD,opens in a new tab or window is an adjunct assistant professor in the department of medicine at Duke University School of Medicine in Durham, North Carolina.
"
Yet Another Issue Is Disrupting the Healthcare Workplace
— Responding to portal messages in "real time" is just the latest assault
by Harry Severance, MD January 10, 2023
Now that patients have online access to their medical information there have been several articles and posts published recently about the increase in patientsopens in a new tab or window seeking -- in real time -- information and explanations about clinical results appearing on their charts. There are also reports now appearing noting that many healthcare facilities are increasingly seeking to billopens in a new tab or window patients for these interactions.
Growing Work Loads: A Case Study
I have been working with one physician colleague concerning evolving changes in his long-standing healthcare workplace and his accelerating feelings of frustration, burnout, and dissatisfaction.
He tells me now that a "final straw" has just been added: real-time health portal messages.
He reports that he used to derive satisfaction from his work, feeling that he was helping people -- the reason, he states, that he sought a career in healthcare. However, the evolving changes in his long-time workplace have now essentially destroyed all that.
Over time, he's seen other changes to his workplace too. The changes began when the facility switched physician contracts to "employee" status. Shortly after, his clinic administrator upped the cap on the number of allowable clinical patient evaluations, first from 4 to 5 per hour and more recently, up to 6 per hour. He told me the per hour cap was originally set based on the complexity and type of patient seen in this clinic. However, in his view the higher caps appear to be an attempt by the facility to increase revenue.
Within the 6 per hour, he reports that usually one to two are new patient evaluations. The facility administration has additionally announced that they expect the majority of interactions to be billed as a "level 3" (or higher).
(A level 3 clinical established follow-up has a typical time of 15 minutesopens in a new tab or window with an actual performance range of 20-29 minutes in 2021, and a new patient E/M level 3 typical time is 30 minutes with the 2021 range averaging 30-44 minutes.)
Six patients each at 15 to 29 minutes per patient, per each 60 minutes? You do the math.
While it's true that administrators frequently overbook clinic visits due to no-show patients who then leave holes in the schedule, this particular clinic has always had a very low percentage of no-shows. This patients per hour computation also does not factor in any additional time for any procedures that might have to be performed.
The physician is also expected, during these time periods, to periodically walk over to an adjacent clinic area to interact with and review the progress of the NP that he is now required to supervise.
He reports that moving to a six patients/hour schedule with these parameters and NP coverage has significantly degraded his ability to keep up, and he reports that his administrator told him recently that she was forced to report him for the increasing delays in patients being seen in a timely fashion in his clinic.
He has attempted multiple times to voice his concerns about these changes to the facility leadership through the appropriate channels, but has not yet even received an acknowledgement, much less a reply to his concerns.
Now, on to the "last straw." Recently, increasing numbers of patients phone calls have been coming into the clinic related to lab tests, imaging studies, and other performance data that this clinic's patients can now access online.
As the number of calls increase and as the facility investigates "billing" for these interactions, he reports that the facility has decided he needs to answer these calls "in real time" as they come in, and take whatever time necessary to fully explain lab and test results to these patients.
Previously, before returning these calls, he had been trying to review and familiarize himself with the report results such as lab tests, or other imaging studies that have been queried -- especially if the results might provide bad news. He would return these calls after his last on-site patient left the clinic, along with the multiple preauthorization peer-to-peer calls he is required to perform with insurance companies.
Yet, despite the new demand to respond right away, he has not been given more time in the clinical schedule to review the information or take the calls. He is still being held to the 6 patients/hour time frame -- and being dinged when he falls behind.
He finds the new approach to these calls profoundly stressful for both him and the patient, and they are leading to distraction and potential loss of focus when he returns to the next on-site patient waiting to be seen. He's concerned this distraction could contribute to medical errors.
He has also tried to share his concerns about increased medical risks with the administration -- but again, with no response.
A Dwindling Workforce
The combination of the increase in patients-per-hour, supervision of mid-level personnel, and now patients calling in during clinical time for results has become, for him, the last straw.
In evaluating his current options, he is not able to migrate to other geographically local facilities due to a non-compete clause he was required to sign when the practicing physicians at his facility were converted to "employee" status, with facilities aggressively attempting to enforce such clauses in his locale.
So, while he felt he was in a previously successful mid-career timeline, he is now considering leaving clinical practice and moving into a non-patient care setting -- or even non-medical setting.
Another good physician (with excellent patient reviews and performance ratings) chewed up by the dystrophic, toxic healthcare workplace. Of course, he's not alone -- too many other doctors and nurses likely feel similarly.
So, it's surprising to me that I am increasingly asked on a regular basis why more and more doctors and nurses are quitting healthcare and why the specter of unionization is starting to appear in the healthcare workplace.
Harry Severance, MD,opens in a new tab or window is an adjunct assistant professor in the department of medicine at Duke University School of Medicine in Durham, North Carolina.
"








![author['full_name'] author['full_name']](https://clf1.medpagetoday.com/media/images/author/Rachael_Robertson_188.jpg)

300x240.png)