- Joined
- Aug 12, 2005
- Messages
- 19,513
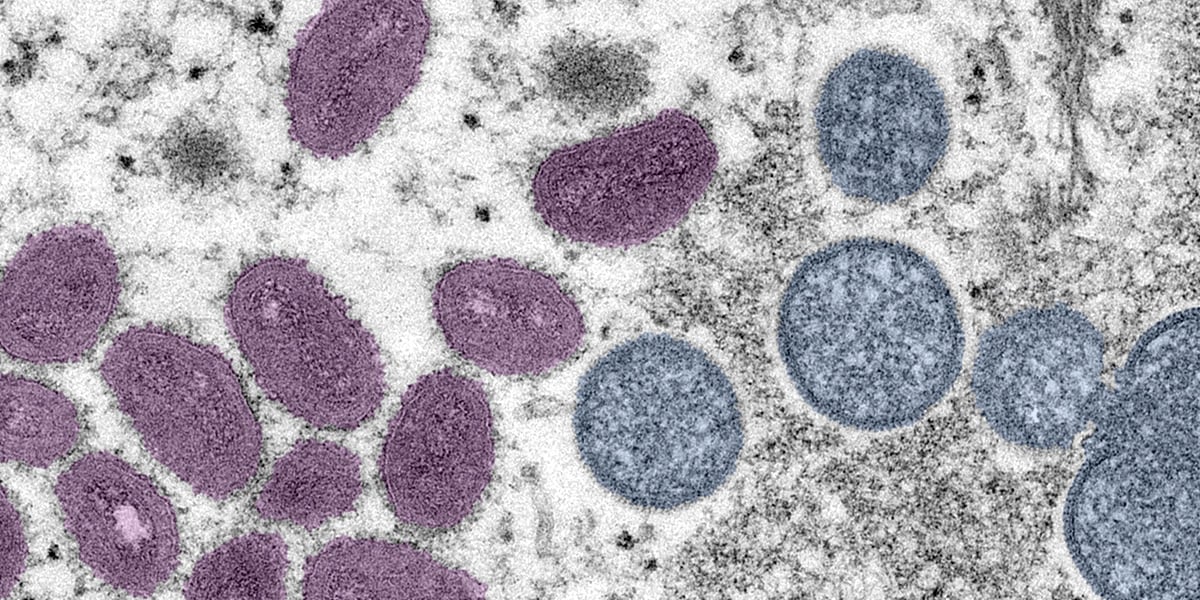
A friend of mine who works in healthcare has me rather concerned about monkey pox and the ease of transmission (air, surfaces, wastewater) as well as a resurgence of polio. No one here is talking about this? I’m surprised…can the medical pros discuss, please? I know that’s a lot to ask; I guess I’m just accustomed to seeing things pop up here before I even hear about them.









300x240.png)